Cornea transplant surgery, which is also referred to as keratoplasty, is a medical procedure that aims to preserve or restore the vision of individuals who have advanced corneal disease or damage. The cornea, which is the clear outer layer of the eye, plays a crucial role in focusing light onto the retina and ensuring clear vision. When the cornea becomes damaged or diseased, it can cause eye pain, blurry vision, and other vision issues. Cornea transplant surgery offers hope to those affected by corneal conditions, giving them an opportunity to regain clear vision and enhance their overall quality of life.
In this comprehensive guide, we will explore the various aspects of cornea transplant surgery, including the reasons for the procedure, different surgical techniques, risks and complications, and the recovery process. Join us as we delve into the world of cornea transplants and discover how this remarkable procedure is transforming lives.
Section 1: Understanding the Cornea
The Cornea: A Window to the World
The cornea is often referred to as the “window to the world” due to its crucial role in allowing light to enter the eye and facilitating clear vision. Located at the front of the eye, the cornea acts as a protective barrier against dirt, germs, and harmful UV light. It works in conjunction with the lens to focus incoming light onto the retina, where visual information is processed and transmitted to the brain.
Common Corneal Conditions and Their Impact
Various conditions can affect the cornea, leading to vision impairment and discomfort. Some of the common corneal conditions include:
- Keratoconus: This condition causes thinning of the cornea, resulting in a cone-shaped protrusion and distorted vision.
- Fuchs’ Dystrophy: Fuchs’ dystrophy is a hereditary condition characterized by the gradual loss of cells in the inner layer of the cornea, leading to corneal swelling and clouding.
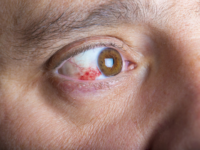
- Corneal Ulcers: Infections can cause the formation of corneal ulcers, which can result in inflammation, scarring, and vision loss.
- Corneal Scarring and Injuries: Traumatic injuries or previous surgeries can cause scarring and damage to the cornea, impairing its clarity and function.
These corneal conditions can significantly impact a person’s ability to see clearly, leading to a diminished quality of life. Cornea transplant surgery offers a potential solution for those whose vision cannot be adequately corrected with glasses, contact lenses, or medications.
Section 2: Reasons for Cornea Transplant Surgery
Restoring Vision and Alleviating Symptoms
Cornea transplant surgery is primarily performed to restore vision and alleviate symptoms in individuals with severe corneal disease or damage. The procedure aims to replace the damaged or diseased cornea with healthy donor tissue, allowing for improved visual acuity and a reduction in discomfort.
Some of the common reasons for cornea transplant surgery include:
- Keratoconus: When the cornea becomes thin and cone-shaped, causing distorted vision and an inability to achieve satisfactory vision correction with glasses or contact lenses.
- Fuchs’ Dystrophy: In cases where Fuchs’ dystrophy progresses to a point where corneal swelling and clouding impact vision significantly.
- Corneal Ulcers: When corneal ulcers fail to respond to medical treatment and cause persistent vision problems.
- Corneal Scarring and Injuries: In situations where corneal scarring or injuries result in significant visual impairment that cannot be corrected through other means.
- Complications from Previous Eye Surgery: When previous eye surgeries lead to corneal complications that affect vision and quality of life.
Cornea transplant surgery offers hope to individuals facing these challenges, providing an opportunity for improved vision and a renewed sense of well-being.
Section 3: Types of Cornea Transplant Surgery
Cornea transplant surgery encompasses several techniques, each tailored to address specific corneal conditions and the extent of corneal damage. The choice of procedure depends on factors such as the layers of the cornea affected and the underlying cause of the corneal condition. Let’s explore some of the most common types of cornea transplant surgery:
Penetrating Keratoplasty: Restoring the Entire Cornea
Penetrating keratoplasty (PK), also known as full-thickness cornea transplant, involves the removal of the entire cornea and replacing it with a healthy donor cornea. This procedure is typically recommended when the entire cornea is affected by severe damage or disease. The surgeon creates a circular incision, removes the damaged cornea, and sutures the donor cornea in place. PK provides a comprehensive solution for restoring vision in cases where the outer, middle, and inner layers of the cornea are compromised.
Deep Anterior Lamellar Keratoplasty: Targeting the Outer and Middle Layers
Deep anterior lamellar keratoplasty (DALK) is a partial-thickness cornea transplant procedure that selectively replaces the outer and middle layers of the cornea while preserving the innermost layer, known as the endothelium. DALK is commonly performed for conditions such as keratoconus or corneal scarring that primarily affect the outer layers of the cornea. By targeting specific layers, DALK reduces the risk of complications associated with full-thickness transplants while achieving desirable visual outcomes.
Endothelial Keratoplasty: Addressing Inner Layer Dysfunction
Endothelial keratoplasty is a specialized cornea transplant technique designed to address conditions that primarily affect the innermost layer of the cornea, known as the endothelium. This procedure aims to replace the dysfunctional endothelial cells with healthy donor cells, promoting corneal clarity and optimal vision. There are two primary types of endothelial keratoplasty:
- Descemet’s Stripping Automated Endothelial Keratoplasty (DSAEK): DSAEK involves removing the damaged endothelial layer and replacing it with a thin layer of donor cornea that includes healthy endothelial cells. This technique provides a smoother recovery and faster visual rehabilitation compared to traditional cornea transplants.
- Descemet’s Membrane Endothelial Keratoplasty (DMEK): DMEK is a more advanced form of endothelial keratoplasty that involves selectively transplanting only the donor’s Descemet’s membrane and endothelial cells. This technique offers even faster visual recovery and improved visual outcomes, with fewer complications.
The choice between DSAEK and DMEK depends on factors such as the extent of endothelial dysfunction and the surgeon’s expertise, ultimately aiming to provide the best possible visual outcomes for each patient.
Section 4: Risks and Complications
As with any surgical procedure, cornea transplant surgery carries potential risks and complications. However, advancements in surgical techniques and post-operative care have significantly reduced the occurrence of complications. It is essential to understand the potential risks involved to make an informed decision about undergoing cornea transplant surgery. Some of the possible risks include:
Rejection of the Transplanted Cornea
The immune system can recognize the transplanted cornea as foreign tissue and mount an immune response, leading to rejection. The risk of rejection is highest within the first year after surgery but can occur at any time. Rejection requires immediate medical attention and can often be managed with medications to suppress the immune response.
Infection
Infection is a potential risk after cornea transplant surgery. The surgical site is susceptible to bacterial, fungal, or viral infections, which can lead to severe complications if left untreated. Close monitoring and adherence to post-operative care instructions, including the use of prescribed medications, help minimize the risk of infection.
Increased Intraocular Pressure
Cornea transplant surgery can occasionally lead to increased intraocular pressure, a condition known as glaucoma. Elevated pressure within the eye can damage the optic nerve and result in vision loss if not properly managed. Regular monitoring and appropriate treatment can help control intraocular pressure and prevent further complications.
Astigmatism and Refractive Errors
Cornea transplant surgery can sometimes lead to astigmatism or refractive errors, causing visual distortions and the need for additional corrective measures such as glasses or contact lenses. These issues can often be addressed through post-operative follow-up care, including the use of specialty lenses or additional surgical interventions if necessary.
Other Potential Complications
Other potential complications of cornea transplant surgery include graft failure, corneal edema, suture-related issues, and delayed wound healing. However, these complications are relatively rare and can often be managed with appropriate medical intervention and follow-up care.
It is crucial to discuss potential risks and complications with your ophthalmologist before undergoing cornea transplant surgery. Your surgeon will provide you with detailed information and guidance to help you make an informed decision about the procedure.
Section 5: Preparing for Cornea Transplant Surgery
Preparation plays a crucial role in ensuring a successful cornea transplant surgery and optimizing the chances of a positive outcome. Your ophthalmologist will guide you through the pre-operative process, which may include:
Comprehensive Eye Examination
Before undergoing cornea transplant surgery, you will undergo a thorough eye examination to assess the health of your eyes and identify any potential issues that may impact the surgery or recovery process. This examination may involve visual acuity tests, corneal topography, and other specialized imaging techniques to evaluate the cornea’s shape, thickness, and overall condition.
Medical Evaluation and Medication Review
Your ophthalmologist will review your medical history, including any underlying health conditions and medications you are currently taking. Certain medications, such as blood thinners, may need to be temporarily discontinued or adjusted before surgery to minimize the risk of bleeding.
Preparing for Other Eye Conditions
If you have any other eye conditions, such as infections or inflammation, these will need to be treated and stabilized before proceeding with cornea transplant surgery. Addressing these conditions beforehand helps optimize the chances of a successful outcome.
Discussion of Expectations and Recovery Process
Your ophthalmologist will discuss the expected outcomes of cornea transplant surgery and provide you with information about the recovery process. It is important to have realistic expectations and understand that visual improvement may take time and vary from person to person.
By following your ophthalmologist’s instructions and preparing adequately for the surgery, you can help ensure a smooth and successful cornea transplant experience.
Section 6: The Cornea Transplant Procedure
Anesthesia and Sedation
Cornea transplant surgery can be performed under local anesthesia or general anesthesia, depending on your specific needs and the surgeon’s recommendation. Local anesthesia numbs the eye area, while general anesthesia allows you to sleep throughout the procedure. Your surgeon will discuss the best option for you based on factors such as your overall health and comfort level.
Cornea Removal and Donor Tissue Placement
During the surgery, your surgeon will make a small incision on the surface of the eye to access the cornea. The damaged or diseased cornea is carefully removed, and the healthy donor cornea is inserted and secured in place using sutures or other techniques. The surgical site is then protected with a patch or shield.
Duration and Recovery
The duration of cornea transplant surgery varies depending on the specific procedure and individual factors. Generally, the surgery takes approximately one to two hours. After the surgery, you will be monitored in a recovery area to ensure stable vital signs and initial healing. Most patients can return home on the same day, although some may require an overnight stay for observation.
Section 7: Post-Operative Care and Recovery
Medications and Eye Drops
Following cornea transplant surgery, your ophthalmologist will prescribe medications to prevent infection, control inflammation, and promote healing. These may include antibiotic and steroid eye drops, as well as oral medications. It is crucial to follow the prescribed medication regimen and attend all post-operative follow-up appointments.
Protecting the Eye and Minimizing Strain
During the initial stages of recovery, it is important to protect the eye and avoid activities that could strain or irritate the surgical site. Your surgeon may recommend wearing a protective shield or eye patch when sleeping or engaging in activities that may pose a risk of eye injury. Avoid rubbing or touching the eye and follow any additional care instructions provided by your healthcare team.
Follow-Up Appointments
Regular follow-up appointments with your ophthalmologist are essential for monitoring the healing process, assessing visual acuity, and addressing any concerns or complications that may arise. Your surgeon will provide a schedule for these appointments, which typically occur in the weeks and months following the surgery.
Gradual Visual Improvement
After cornea transplant surgery, it is important to understand that visual improvement is a gradual process. It may take several months or even up to a year to achieve optimal visual acuity. Be patient and communicate any changes or concerns to your healthcare team during the recovery period.
Section 8: Success Rates and Long-Term Outcomes
Cornea transplant surgery has a high success rate, with most patients experiencing significant improvement in vision and a reduction in symptoms. The success of the procedure depends on various factors, including the underlying condition, the surgical technique employed, and the individual’s overall health.
Long-term outcomes of cornea transplant surgery are generally favorable, with transplanted corneas lasting for many years. However, it is important to continue regular follow-up appointments to monitor the health of the transplanted cornea and ensure early detection of any potential complications.
Section 9: The Gift of Cornea Donation
Cornea transplant surgery would not be possible without the generous act of cornea donation. Donated corneas come from individuals who have chosen to give the gift of sight after their passing. The donated corneas undergo thorough testing and screening to ensure their safety and suitability for transplantation.
If you are interested in donating your corneas or learning more about the donation process, consider registering as an organ donor in your country. By doing so, you can make a significant impact on someone’s life by restoring their vision and improving their quality of life.
Section 10: Conclusion
Cornea transplant surgery is a remarkable procedure that offers hope to individuals with corneal disease or damage. By replacing the damaged cornea with healthy donor tissue, this surgery can restore vision, alleviate symptoms, and improve the overall quality of life for many patients.
If you or a loved one is considering cornea transplant surgery, it is essential to consult with an experienced ophthalmologist who can guide you through the process and provide personalized care. By understanding the benefits, risks, and recovery process associated with cornea transplant surgery, you can make an informed decision and embark on a journey towards restored vision and improved well-being.