Hey there, sinus sufferers! If you’ve been dealing with chronic rhinosinusitis and find yourself constantly reaching for tissues, you’re in the right place. In this blog post, we’re going to dive into the fascinating world of inflammation and its role in this pesky condition. Chronic rhinosinusitis, or CRS for short, is a common inflammatory disorder that affects the nasal passages and sinuses. But have you ever wondered why inflammation plays such a pivotal role in this condition? Well, stick around because we’re going to explore the pathophysiological mechanisms behind it all. So grab a cup of tea, get cozy, and let’s unravel the mysteries of CRS and the role inflammation plays in it!
Introduction to Chronic Rhinosinusitis
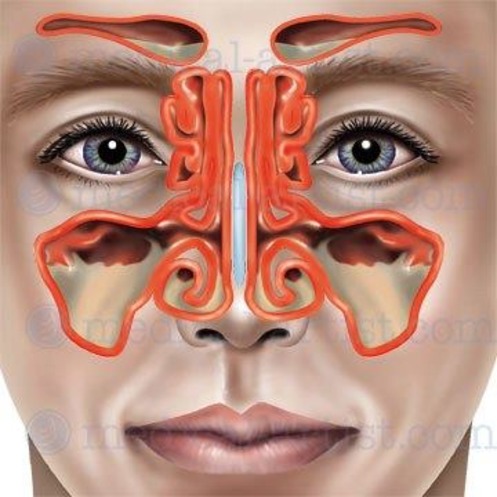
The pathophysiology of chronic rhinosinusitis (CRS) revolves around the persistent inflammation and swelling that occur in the sinus and nasal passages. This common, chronic condition is marked by the gradual development of inflammation in these areas, leading to various symptoms such as nasal congestion, facial pain, and difficulty breathing through the nose. The underlying mechanisms behind CRS involve a complex interplay of factors including immune responses, bacterial or fungal infections, anatomical abnormalities, and environmental triggers. The chronic inflammation results in the thickening of the sinus mucosa, impaired mucus clearance, and the formation of nasal polyps in some cases. These processes contribute to the obstructive nature of CRS, causing persistent discomfort and even complications if left untreated. Understanding the pathophysiology of chronic rhinosinusitis provides valuable insights for both the management and prevention of this condition, emphasizing the need for a comprehensive approach that addresses the different aspects contributing to its development.
Chronic rhinosinusitis pathophysiology involves various factors that contribute to the development and progression of the condition. One important aspect of this pathophysiology is the potential obstruction of the natural drainage pathways of the sinuses. This obstruction can occur due to factors such as nasal polyps, deviated septum, or other anatomical abnormalities. When these drainage pathways are obstructed, it can lead to impaired sinus ventilation, preventing proper airflow within the sinuses. As a consequence, mucus production in the sinuses increases, creating an ideal environment for the growth of bacteria and other microorganisms. This increased mucus production further aggravates the obstruction, perpetuating a cycle of inflammation and worsening symptoms for individuals suffering from chronic rhinosinusitis. Understanding the intricate mechanisms involved in chronic rhinosinusitis pathophysiology is crucial in developing effective treatment strategies aimed at addressing the underlying causes and relieving symptoms for patients.
Chronic rhinosinusitis pathophysiology encompasses a range of symptoms that can significantly affect an individual’s quality of life. One of the key manifestations of this condition is the experience of facial pain or pressure, which can be persistent and debilitating. Furthermore, patients with chronic rhinosinusitis pathophysiology often suffer from nasal congestion, which can make breathing difficult and lead to a feeling of constant stuffiness. Another common symptom is post-nasal drip, where mucus drips down the back of the throat, causing throat irritation and persistent coughing. Additionally, individuals with this condition may experience a loss of smell or taste, as the chronic inflammation in the sinuses can interfere with these sensory functions. These symptoms, collectively affecting patients with chronic rhinosinusitis pathophysiology, underscore the need for effective treatment options to alleviate the burden that this condition places on individuals.
Moreover, understanding the pathophysiology of chronic rhinosinusitis is crucial for developing effective treatment options. Inflammation plays a central role in CRS, leading to impaired sinus drainage and the persistence of symptoms. By targeting the underlying inflammation, treatment approaches aim to alleviate symptoms and improve sinus drainage. Medications such as corticosteroids, antibiotics, and nasal irrigation have shown promise in reducing inflammation and restoring normal sinus function. Additionally, surgical interventions may be considered for patients with severe or refractory cases of CRS, aiming to remove obstructions and create optimal sinus drainage. Overall, a comprehensive understanding of chronic rhinosinusitis pathophysiology is vital in guiding treatment decisions and providing relief to individuals suffering from this debilitating condition.
Causes of Inflammation in Chronic Rhinosinusitis
The pathophysiology of chronic rhinosinusitis revolves around inflammation, which is the primary cause of this condition. Chronic rhinosinusitis pathophysiology involves the persistent and prolonged inflammation within the sinuses and nasal passages. This inflammation leads to the swelling of these structures, causing discomfort and difficulty in breathing. Inflammation in chronic rhinosinusitis pathophysiology is a complex process involving various immune cells and inflammatory mediators. The immune cells, such as neutrophils and eosinophils, infiltrate the nasal mucosa and sinuses, releasing pro-inflammatory substances. These substances further promote the recruitment of more immune cells, perpetuating the inflammatory response. The swelling resulting from chronic rhinosinusitis pathophysiology can obstruct the drainage pathways, leading to mucus accumulation and bacterial overgrowth. This environment provides a favorable breeding ground for infections and exacerbates the inflammatory response. Understanding the pathophysiology of chronic rhinosinusitis is crucial for developing effective treatment strategies that target the underlying inflammation. By addressing the inflammation at its core, healthcare professionals can alleviate symptoms and improve the quality of life for individuals with chronic rhinosinusitis.
Chronic rhinosinusitis pathophysiology involves a complex interplay of various factors that contribute to the inflammation of the nasal cavity. Allergies, environmental irritants, infections, and structural issues within the nasal cavity are key contributors to this condition. When individuals with chronic rhinosinusitis are exposed to allergens or irritants, their immune system reacts by triggering inflammation in the nasal cavity. This inflammation can be further exacerbated by infections, which can lead to increased mucus production and blockage of the sinus passages. Additionally, structural abnormalities within the nasal cavity, such as deviated septum or nasal polyps, can also impede proper sinus drainage and ventilation, further promoting inflammation. Understanding the chronic rhinosinusitis pathophysiology is crucial in developing effective treatment strategies to alleviate symptoms and improve the overall quality of life for affected individuals.
All in all, understanding the pathophysiology of chronic rhinosinusitis (CRS) is crucial in developing effective treatment strategies. The multifactorial nature of CRS involves various mechanisms, including the role of inflammation. In particular, the presence of inflammation is seen as a major contributor to the persistence of CRS symptoms. The overexpression of proinflammatory cytokines and chemokines, as well as the infiltration of immune cells, perpetuate the inflammatory response in CRS. Furthermore, certain medications, such as non-steroidal anti-inflammatory drugs (NSAIDs), may also contribute to inflammation in CRS by further aggravating existing inflammation or inducing new areas of inflammation. Therefore, by understanding the complex interplay between inflammation and CRS, healthcare professionals can tailor treatment plans that address both the underlying pathophysiological processes and specific patient needs, ultimately improving the management and outcomes of this chronic condition.
Role of Allergens and Infections in Chronic Rhinosinusitis Pathophysiology
The pathophysiology of chronic rhinosinusitis involves a complex interplay between allergens and infectious agents. Inflammation of the nose and sinuses, which characterize this condition, can be triggered by both allergens and infections. Allergens such pollen, dust mites, and pet dander can initiate an immune response in susceptible individuals, leading to chronic inflammation in the nasal and sinus passages. On the other hand, infections caused by bacteria, viruses, or fungi can directly invade the sinuses, causing inflammation and exacerbating the symptoms of chronic rhinosinusitis. The presence of both allergens and infectious agents further amplifies the inflammatory response, resulting in persistent symptoms. Therefore, understanding the comprehensive role of both allergens and infections is crucial in managing the pathophysiology of chronic rhinosinusitis.
Chronic rhinosinusitis pathophysiology is primarily characterized by allergic inflammation, which occurs when an individual is exposed to certain allergens, such dust mites or animal dander. This exposure triggers the release of histamine from mast cells, resulting in various symptoms associated with chronic rhinosinusitis. Increased mucus production and nasal congestion are common outcomes of this process, often accompanied by frequent sneezing. These symptoms collectively contribute to the overall pathophysiology of chronic rhinosinusitis, highlighting the complex immune and inflammatory responses that occur in the nasal and sinus passages. Understanding this underlying mechanism is crucial in developing effective treatment strategies to alleviate the discomfort and improve the quality of life for individuals affected by chronic rhinosinusitis.
Again, understanding the pathophysiology of chronic rhinosinusitis is crucial in comprehending the complex nature of the disease. Infections play a significant role in the development of chronic rhinosinusitis, particularly when bacteria or viruses invade the sinuses, triggering inflammation and obstructing the sinus passages. The resulting blockage gives rise to persistent symptoms such headache, facial pain, cough, fever, and nasal discharge. Recognizing the interplay between infections and the breakdown of normal sinus functioning sheds light on the intricacies of chronic rhinosinusitis pathophysiology. By delving deeper into this understanding, researchers and healthcare professionals can strive to develop more effective treatments and management strategies for those suffering from this chronic condition.
Interactions Between Airway Mucosal Cells and the Immune System
The pathophysiology of chronic rhinosinusitis (CRS) involves multiple factors, one of which is the role of mucosal cells. These cells serve a crucial function by acting the primary interface between environmental pathogens and the immune system in CRS. By interacting with pathogens present in the nasal and sinus cavities, mucosal cells play a pivotal role in mediating the immune response. In CRS, the dysfunction of these cells can contribute to the perpetuation of inflammation and the impaired clearance of pathogens. Understanding the intricate mechanisms behind mucosal cell function and its interactions with environmental pathogens is therefore vital in comprehending the pathophysiology of CRS and developing targeted therapeutic interventions.
Chronic rhinosinusitis, a chronic inflammatory disorder affecting the sinuses and nasal passages, is characterized by the abnormal inflammation of the airway mucosal cells. These cells play a crucial role in recognizing potential pathogens through toll-like receptors, which are capable of activating a range of innate immune responses. One such response includes the initiation of inflammation within the affected area. Additionally, these receptors also induce the production of cytokines, which are essential for modulating immune responses and mediating communication between immune cells. The activation of toll-like receptors in airway mucosal cells during chronic rhinosinusitis pathophysiology amplifies the inflammatory response and enhances cytokine production, contributing to the chronic nature of the disease. Understanding these key mechanisms is vital for developing effective therapeutic strategies that target the underlying mechanisms of chronic rhinosinusitis and help alleviate symptoms in affected individuals.
Finally, chronic rhinosinusitis (CRS) pathophysiology involves a complex interplay of various molecules, including cytokines, chemokines, histamine, and leuko-trienes. This orchestrated inflammatory response triggers the recruitment of immune cells into the airways of CRS sufferers, leading to a never-ending cycle of persistent airway inflammation. The presence of these key keywords emphasizes the significance of these molecules in the pathogenesis of CRS and highlights their role in perpetuating the disease process. This understanding underscores the importance of targeted therapies that aim to modulate this inflammatory response and restore normal immune function in order to alleviate symptoms and improve the quality of life for individuals afflicted with CRS.
Types of Inflammation Involved in Chronic Rhinosinusitis
Chronic rhinosinusitis pathophysiology is characterized by a persistent inflammation of the sinuses and nasal cavities. This condition can be triggered by various factors, including environmental allergens, viral infections, bacteria, or a combination of these agents. The underlying mechanisms of chronic rhinosinusitis pathophysiology involve an abnormal immune response, leading to inflammation and tissue damage in the sinuses and nasal passages. The immune system reacts to the presence of allergens, viruses, or bacteria by releasing inflammatory mediators, such histamines and cytokines. These mediators cause blood vessel dilation, increased mucus production, and recruitment of immune cells to the affected area. Consequently, the lining of the sinuses becomes swollen and congested, impeding proper airflow and drainage. Additionally, the excessive mucus production contributes to the formation of nasal polyps and obstructed sinuses, further exacerbating the symptoms of chronic rhinosinusitis. Understanding the intricate pathophysiological processes involved in chronic rhinosinusitis is crucial for developing effective treatment strategies aimed at reducing inflammation, improving sinus drainage, and alleviating patient discomfort.
Chronic rhinosinusitis pathophysiology encompasses the involvement of two distinct types of inflammation, namely eosinophilic and neutrophilic inflammation. Eosinophilic inflammation manifests through the infiltration of eosinophils within the tissue and the subsequent metastasis of these cells into the lumen of the sinus cavities. This particular aspect plays a crucial role in understanding the underlying mechanisms of chronic rhinosinusitis pathophysiology. By recognizing the prevalence and characteristics of eosinophilic inflammation, healthcare professionals can better comprehend the intricate nature of this condition and develop targeted treatment strategies. Understanding the specific types of inflammation involved in chronic rhinosinusitis pathophysiology is vital in providing comprehensive care and improving patient outcomes.
The pathophysiology of chronic rhinosinusitis involves various mechanisms, one of which is neutrophilic inflammation. This specific type of inflammation is characterized by an excessive infiltration of neutrophils into the paranasal sinuses and surrounding tissues. As a result, there is an accumulation of inflammatory mediators that not only exacerbates existing tissue damage but also contributes to the progression of chronic rhinosinusitis. This phenomenon plays a crucial role in the overall pathophysiology of chronic rhinosinusitis, highlighting the importance of understanding and targeting neutrophilic inflammation in the development of effective treatment strategies for this condition.
Meanwhile, understanding the pathophysiology of chronic rhinosinusitis becomes increasingly complex due to the coexistence of both types of inflammation in CRS patient populations. This dual nature of inflammation poses a significant challenge in identifying and targeting specific pathways for effective treatment. The intricate interaction between various factors within the nasal and sinus mucosa further complicates the pathophysiological mechanisms at play. Although there have been advancements in our understanding of chronic rhinosinusitis pathophysiology, much remains to be elucidated. Continued research and exploration into the underlying molecular and cellular mechanisms of CRS are crucial for the development of targeted and personalized therapeutic interventions to provide relief and improve the quality of life for affected individuals.
Role of Neurogenic Inflammation in Chronic Rhinosinusitis
Chronic rhinosinusitis pathophysiology encompasses various complex mechanisms that contribute to the development and persistence of this condition. One significant aspect is neurogenic inflammation, a distinct form of inflammation observed in chronic rhinosinusitis (CRS). This particular type of inflammation involves the release of neuropeptides from sensory nerves situated within the sinonasal mucosa. These neuropeptides are triggered by either inflammation or mechanical trauma, and their release exacerbates the inflammatory response in CRS. The activation of sensory nerves in the sinonasal mucosa plays a crucial role in perpetuating the inflammation and symptoms associated with chronic rhinosinusitis. Understanding the role of neurogenic inflammation is imperative for comprehending the pathophysiology of CRS and devising effective treatment strategies that target this specific mechanism.
Chronic rhinosinusitis pathophysiology is a complex subject that has been extensively researched, revealing important insights into the underlying mechanisms of this condition. One significant finding is the presence of neurogenic inflammation, which has been shown to play a crucial role in the development and progression of chronic rhinosinusitis. This type of inflammation is associated with several detrimental effects on nasal health, such an increase in vascular permeability, heightened mucus secretion, and smooth muscle contraction. These changes can ultimately lead to nasal obstruction and impair the natural clearance of mucus, further exacerbating the symptoms of chronic rhinosinusitis. Understanding these aspects of chronic rhinosinusitis pathophysiology is crucial for developing effective treatments and improving the quality of life for individuals affected by this condition.
Moreover, understanding the pathophysiology of chronic rhinosinusitis (CRS) is crucial in order to effectively manage and treat this debilitating condition. Neurogenic inflammation, specifically in the sinonasal mucosa, has emerged not only to be linked to pain perception, but also to play a pivotal role in the patient’s overall experience of disease burden and exacerbations of CRS symptoms during acute inflammation. The recognition of neurogenic inflammation’s association with pain perception in CRS provides valuable insights into potential therapeutic targets and interventions that could significantly improve patient outcomes. By addressing the underlying mechanisms involved in neurogenic inflammation, clinicians and researchers can strive towards more precise and personalized treatment strategies, ultimately alleviating the pain and burden associated with CRS, and enhancing the quality of life for affected individuals.
Impact of Mediators on the Pathophysiology of Chronic Rhinosinusitis
Chronic rhinosinusitis pathophysiology is a complex phenomenon that encompasses various inflammatory processes within the nasal passages and sinuses. This common disorder, known specifically by its abbreviation CRS, is characterized by the persistent inflammation of the mucosa. As a result of this chronic inflammation, the normal mechanisms responsible for mucociliary clearance – the process of removing mucus and debris from the nasal passages – become disrupted. Additionally, the impaired drainage within the sinuses further contributes to the overall pathophysiology of chronic rhinosinusitis. Understanding these underlying mechanisms is vital in order to develop effective treatments and interventions for individuals suffering from this condition.
In the pathophysiology of chronic rhinosinusitis, immune cells play a crucial role in the inflammatory process within the sinonasal cavity. Mediators, including cytokines, chemokines, eicosanoids, and growth factors, are released by these immune cells from both the epithelium and the lamina propria. These mediators contribute significantly to the ongoing inflammation observed in chronic rhinosinusitis. The release of these inflammatory mediators further exacerbates the underlying pathophysiological mechanisms associated with chronic rhinosinusitis, perpetuating the inflammatory cascade and contributing to the persistence of symptoms in affected individuals. Understanding the intricate involvement of these mediators is key to comprehending the complex nature of chronic rhinosinusitis pathophysiology and may provide potential targets for therapeutic interventions aimed at managing this debilitating condition.
Furthermore, the dysregulation of cytokines such interleukin-8, tumor necrosis factor alpha, interferon gamma, and other mediators in chronic rhinosinusitis pathophysiology is not only a consequence but also a perpetuating factor of the disease. These inflammatory molecules have been found to be significantly upregulated in CRS, contributing to the relentless cycle of inflammation and structural damage within the sinuses. Through their actions, these cytokines can further exacerbate symptomatology associated with CRS, creating a vicious cycle that is challenging to break. Understanding the role of these cytokines in chronic rhinosinusitis pathophysiology is crucial for developing targeted therapeutic strategies aimed at controlling inflammation and ultimately improving patient outcomes.
Interplay Between Immune Response and Infection in Chronic Rhinosinusitis
Chronic rhinosinusitis, a persistent inflammatory condition affecting the sinonasal mucosa, is characterized by a complex interaction between immune response and infection. The pathophysiology of this condition revolves around the intricate dynamics between the immune system and the presence of infectious agents. The immune response initiates an inflammatory cascade, leading to the activation of immune cells and release of various mediators. This inflammatory process damages the sinonasal mucosa, disrupt normal respiratory functions, and perpetuates a cycle of chronic inflammation. Simultaneously, infections play a significant role in exacerbating this condition, either by triggering the immune response or by providing a constant source of antigenic stimulation. Understanding the pathophysiology of chronic rhinosinusitis is crucial for effective management and the development of targeted therapeutic approaches. By unraveling the intricate mechanisms underlying this disorder, researchers and healthcare professionals can strive for improved treatment outcomes, aimed at alleviating inflammation, combating infections, and restoring normal sinonasal function.
Chronic rhinosinusitis, a condition within the field of chronic rhinosinusitis pathophysiology, is characterized by the occurrence of an overactive immune response coinciding with bacterial or viral infections. This interaction leads to the development of airway inflammation and obstruction, key elements in the pathophysiology of this condition. The immune system, in its overactivity, responds excessively to these infections, triggering a cascade of events that result in the inflammation and blockage of the airways. The chronic nature of this condition means that these symptoms persist over an extended period, causing significant discomfort and impairing daily functioning. By understanding the underlying mechanisms involved in chronic rhinosinusitis pathophysiology, researchers and healthcare professionals can better tailor treatment approaches to mitigate symptoms and improve the quality of life for individuals affected by this condition.
Chronic rhinosinusitis is a complex condition characterized by persistent inflammation in the nasal cavity and sinuses. The pathophysiology of this condition involves various mechanisms that ultimately contribute to the development of its symptoms. One key aspect is the inflammation, which results in the thickening of the mucosal lining. This thickening not only narrows the passageways, causing congestion, but also disrupt the normal functioning of the cilia. The cilia are tiny hair-like structures that line the nasal cavity and usually work to clear debris and infectious particles from the airways. However, in chronic rhinosinusitis, their function becomes impaired due to the inflammation. This impaired cilia function further contributes to the accumulation of mucus and obstructed airways. Additionally, the inflammation triggers an overproduction of mucus, exacerbating the congestion and resulting in a persistent feeling of nasal blockage. Understanding the pathophysiology of chronic rhinosinusitis is crucial for developing effective treatment strategies that aim to alleviate inflammation, restore ciliary function, and reduce mucus production, providing relief to individuals suffering from this condition.
Thus, understanding the chronic rhinosinusitis pathophysiology is crucial in comprehending the complex immune response-infection mechanism that perpetuates the ongoing inflammation in the sinuses. This intricate interaction between the immune system and infectious agents leads to a variety of distressing symptoms for the patient. These symptoms, including facial pain, nasal congestion, postnasal drip, headaches, and difficulty breathing through the nose for extended periods of time, can significantly impact an individual’s quality of life. By delving into the pathophysiology of chronic rhinosinusitis, researchers and healthcare professionals can gain valuable insights that may ultimately lead to more effective treatment strategies and improved outcomes for affected individuals.
Conclusions Regarding the Role of Inflammation in Chronic Rhinosinusitis
Chronic rhinosinusitis pathophysiology is an intricate subject that involves multiple risk factors contributing to the development of this condition. One key factor is chronic inflammation of the sinonasal mucosa, which plays a critical role in the pathogenesis of chronic rhinosinusitis. This persistent inflammation within the nasal and sinus cavities can lead to various changes in the mucosal lining, suchas increased vascular permeability and mucus production, ultimately resulting in the characteristic symptoms of chronic rhinosinusitis. Furthermore, these alterations can impair the normal clearance mechanisms of the respiratory tract, leading to the colonization of bacteria or fungi and the perpetuation of the inflammatory response. Additionally, other factors suchas genetics, environmental factors, and immunological abnormalities may also contribute to the pathophysiology of chronic rhinosinusitis. Understanding the complex mechanisms and risk factors involved in this condition is crucial for developing effective treatment strategies tailored to individual patient needs.
The pathophysiology of chronic rhinosinusitis is thought to be closely linked to inflammatory processes, based on various studies. These investigations have shown that there is an evident increase in the levels of pro-inflammatory mediators in the sinonasal mucosa, indicating their significant role in this condition. Moreover, elevated levels of inflammatory cytokines in the serum further support the involvement of inflammatory processes in the pathophysiology of chronic rhinosinusitis. These findings provide valuable insights into the underlying mechanisms of this condition, highlighting the importance of understanding chronic rhinosinusitis pathophysiology for effective management and treatment strategies.
Furthermore, in the context of chronic rhinosinusitis pathophysiology, it is crucial to consider the involvement of both systemic and local immunomodulation in the progression or persistence of this condition. Recent research has shed light on the significance of these mechanisms in understanding the complex nature of chronic rhinosinusitis. The term immunomodulation refers to the ability to modify or regulate immune responses. It has been found that various factors, both within the body and in the immediate environment, can influence the immune system’s activities in the sinuses and nasal passages. This can have a substantial impact on the development and progression of chronic rhinosinusitis. Systemic immunomodulation refers to how the entire immune system functions throughout the body, while local immunomodulation focuses specifically on the immune response within the sinuses and nasal passages themselves. By exploring these aspects of immunomodulation, researchers are gaining a deeper understanding of the underlying processes contributing to chronic rhinosinusitis. This knowledge is crucial for developing effective treatments and interventions that target these immune-mediated mechanisms at both systemic and local levels. Therefore, a comprehensive examination of immunomodulation is pivotal in unraveling the complexities of chronic rhinosinusitis pathophysiology and paving the way for improved patient outcomes.
Furthermore, the evidence presented in this study strongly supports the notion that inflammation plays a pivotal role in the development and progression of chronic rhinosinusitis. By focusing on targeting inflammation, clinicians and researchers may be able to develop more effective management strategies and treatments for this debilitating condition. Future studies should aim to further elucidate the specific mechanisms and pathways involved in the pathophysiology of chronic rhinosinusitis and explore novel therapeutic approaches that directly address inflammation. By doing so, we can hope to alleviate the burden of chronic rhinosinusitis for affected individuals, improving their quality of life and overall well-being.
Read also: Clinically Relevant Phenotypes in Chronic Rhinosinusitis
In conclusion, understanding the role of inflammation in chronic rhinosinusitis (CRS) is crucial for both patients and healthcare professionals alike. By delving into the pathophysiological mechanisms behind this condition, we have discovered the intricate relationship between inflammation and CRS. From the activation of inflammatory cells to the release of various inflammatory mediators, it is clear that inflammation is deeply intertwined with the development and persistence of symptoms in CRS. Recognizing this pivotal role opens up avenues for new treatment strategies that target inflammation directly, offering hope for effective management and improved quality of life for those affected by this pesky condition. So next time you find yourself constantly reaching for tissues, know that a deeper understanding of inflammation can lead to better outcomes in your journey towards finding relief from chronic rhinosinusitis.