Hey there, fellow stuffy nose sufferers! If you’ve ever found yourself desperately trying to breathe through your congested nasal passages, then you know just how frustrating and uncomfortable nasal congestion can be. Whether it’s due to a seasonal allergy attack or a nasty cold, having a clogged nose is no fun at all. That’s why we’ve put together this comprehensive guide to help you understand the five most common causes of nasal congestion. From allergies to sinus infections, we’ll dive into the nitty-gritty details, explaining what exactly causes that annoying blockage and how you can find some much-needed relief. So, sit back, relax, and get ready to bid farewell to that stubborn stuffiness once and for all!
Overview of Pathophysiology of Nasal Congestion
The pathophysiology of nasal congestion, also referred to colloquially
as a stuffy nose, can be attributed to various factors. One prominent cause is upper respiratory infections triggered by viruses or allergens. In these cases, the nasal cavities’ tissues undergo inflammation and swelling due to an increase in fluid retention. Consequently, airflow becomes obstructed, posing challenges in breathing through the nose. Nasal congestion often presents itself with discomfort and difficulty, hindering everyday activities and causing significant inconvenience. Understanding the pathophysiology behind this common symptom is crucial for developing effective treatment strategies.
The pathophysiology of nasal congestion involves a range of symptoms that can be associated with this condition. In some cases, individuals may experience not only nasal congestion but also related symptoms such facial pressure or pain, watery eyes, sneezing, sore throat, post-nasal drip, a runny nose, and headaches. These symptoms collectively contribute to the overall discomfort and inconvenience of nasal congestion. Nasal congestion occurs when there is swelling and inflammation of the nasal passages, usually due to a common cold, allergies, or sinus infections. This inflammation leads to a blockage in the flow of air through the nose, causing a feeling of stuffiness and congestion. Understanding the pathophysiology of nasal congestion allows healthcare professionals to better identify and manage this condition, alleviating its symptoms and improving the quality of life for affected individuals.
In conclusion, the pathophysiology of nasal congestion is complex, with various underlying causes that can contribute to its development. Viral or bacterial infections, allergies, and exposure to environmental irritants such smoke or dust mites are common factors that can trigger nasal congestion. Understanding the pathophysiology of this condition is crucial for effective treatment. Depending on the severity of the congestion, individuals may opt for over-the-counter medications and home remedies, or seek more advanced medical interventions. It is essential to address this uncomfortable symptom promptly to alleviate discomfort and improve quality of life. By acknowledging and addressing the underlying causes of nasal congestion, appropriate treatment can be pursued, leading to relief and improved respiratory health.
Pathophysiology of Nasal Congestion
The pathophysiology of nasal congestion revolves around the inflammation occurring in the mucus membranes of the nasal passages. Nasal congestion is a prevalent symptom associated with various illnesses, characterized by the swelling and blockage of the nasal passages. This inflammation arises mainly from two causes – an allergic reaction or an infection, suchas the common cold. Allergens trigger an immune response, leading to the release of histamines, which results in the swelling of the mucus membranes. Infections, on the other hand, stimulate the body’s immune system to release cytokines, causing inflammation in the nasal passages. Understanding the pathophysiology of nasal congestion is crucial for diagnosing and treating the underlying causes effectively.
The pathophysiology of nasal congestion involves the body’s inflammatory response, which initiates a series of events. This response leads to the swelling of the nasal mucosa, causing a reduction in airflow through the nose. Additionally, this swelling triggers an increase in mucus production, further obstructing the nasal passage and impeding proper breathing. The inflammation-induced irritation can also result in troublesome symptoms such coughing, sneezing, and other discomforting effects. These include a runny nose, post-nasal drip, and itchy and watery eyes. Overall, the pathophysiology of nasal congestion involves a complex chain of reactions influenced by the body’s inflammatory response, leading to various distressing symptoms that impact daily life.
Meanwhile, understanding the pathophysiology of nasal congestion is crucial in developing effective treatment strategies. In order to alleviate the symptoms associated with nasal congestion, such
as stuffiness and difficulty breathing, a combination of decongestant medications and antihistamines is commonly prescribed. These medications work by reducing the swelling of the nasal passages and minimizing allergic reactions that may contribute to or worsened congestion. Additionally, over-the-counter saline rinses can be utilized to alleviate inflammation and enhance the flow of air through the nasal passages. By addressing the underlying pathophysiology of nasal congestion, healthcare providers can ensure that patients receive appropriate and tailored treatment options for this common condition.
Common Causes of Nasal Congestion
Nasal congestion, a common symptom experienced by many individuals, can be attributed to various causes related to the pathophysiology of nasal congestion. The primary culprits are viral infections like the common cold and influenza, which lead to inflammation of the nasal passages, resulting in blockage and discomfort. Additionally, environmental irritants such dust or smoke can also trigger nasal congestion by irritating the delicate nasal tissues, causing swelling and obstruction. Allergies to substances such pollen, pet dander, or other allergens are another significant contributor to nasal congestion. When exposed to these allergens, the body’s immune system reacts by producing histamines, which cause the nasal blood vessels to dilate and increase mucus production, leading to congestion. Understanding the pathophysiology of nasal congestion helps in comprehending the underlying mechanisms behind this frustrating symptom and finding appropriate treatments to alleviate discomfort.
Nasal congestion, a common symptom in the pathophysiology of various allergies, can be triggered by allergens such pollen, pet dander, and other substances. When an individual with a sensitivity to these allergens comes into contact with them, the immune system responds by releasing histamine. This histamine release serves to protect the body from potential harm, but in the case of allergies, it can cause an inflammatory response in the nose. This inflammation leads to swelling and blockage of the nasal passages, resulting in the unpleasant sensation of nasal congestion. The presence of histamine promotes increased blood flow to the affected area, which further contributes to the congestion. Therefore, understanding the role of histamine in the development of nasal congestion is crucial in comprehending the pathophysiology of this bothersome symptom.
Nasal congestion, a common symptom experienced during viral infections such asthe common cold, is closely linked to the pathophysiology of inflammation in the nasal passages. Viral infections can trigger an inflammatory response in the tissue lining the nasal passages, causing it to become swollen. This swelling, combined with increased mucus production, can lead to a narrowing or even complete blockage of the airways. As a result, individuals may experience nasal congestion, making it difficult to breathe through their nose. Understanding the pathophysiology of nasal congestion provides valuable insights into the underlying mechanisms that contribute to this uncomfortable symptom.
However, it is important to note that the pathophysiology of nasal congestion is a complex and multifactorial process. While environmental irritants such dust or smoke can certainly contribute to the swelling and increased mucus production in the nasal passages, they are not the sole culprits. Numerous other factors, such allergies, infections, and structural abnormalities, can also play a significant role in the development and persistence of nasal congestion. Understanding the underlying mechanisms of this condition requires a careful examination of these various factors and their interactions. By gaining a comprehensive understanding of the pathophysiology of nasal congestion, healthcare professionals can better tailor their treatment approaches and provide relief for individuals who suffer from this bothersome condition.
The pathophysiology of nasal congestion is a complex process that can be classified into three main sub-headings: inflammatory, structural, and infectious. Inflammatory causes of nasal congestion involve the body’s immune response to irritants or allergens in the nasal passages. This response leads to swelling of the nasal mucosa, increased mucus production, and narrowing of the nasal airways. Structural factors contributing to nasal congestion include anatomical abnormalities, such a deviated nasal septum or nasal polyps, which can obstruct the flow of air through the nose. Lastly, infectious causes of nasal congestion arise from viral or bacterial infections that result in inflammation of the nasal passages. These infections commonly produce symptoms such a stuffy nose, sinus pressure, and nasal discharge. Understanding these different aspects of the pathophysiology of nasal congestion is essential for proper diagnosis and management of this common condition.
The pathophysiology of nasal congestion relates to the underlying mechanisms that contribute to the condition. There are several inflammatory causes that can lead to nasal congestion, which in turn affects an individual’s ability to breathe comfortably. Allergies, for instance, trigger an inflammatory response in the nasal passages, causing swelling and congestion. Similarly, chronic sinusitis, characterized by persistent inflammation of the sinuses, can result in nasal congestion. Colds and flus can also lead to congestion by causing inflammation in the respiratory system. Moreover, environmental factors such pollution or smoke can act irritants, promoting nasal congestion through inflammation. Understanding the pathophysiology behind nasal congestion is crucial for effective management and treatment of this common condition.
The pathophysiology of nasal congestion involves various structural causes that can significantly impact the airways and result in blocked nasal passages. One of these causes is a deviated septum, where the thin wall separating the nostrils is displaced to one side, obstructing the free flow of air. This misalignment can contribute to chronic nasal congestion, making it difficult for individuals to breathe comfortably through their nose. Another structural cause is the presence of nasal polyps, which are soft, non-cancerous growth that can develop in the lining of the nasal passages. These polyps may gradually increase in size, causing further blockage of the airways and exacerbating nasal congestion. Recognizing these keywords, it becomes evident that understanding the pathophysiology of nasal congestion entails considering these structural factors that can impede airflow and result in discomfort for affected individuals.
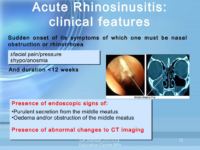
The pathophysiology of nasal congestion involves various infectious causes, primarily triggered by viral or bacterial infections. These infections can be commonly associated with ailments like the common cold, flu, sinus infection, or streptococcal throat infection. Nasal congestion occurs when there is inflammation and swelling of the nasal tissues, resulting in a blocked or stuffy nose. Viral infections, such the common cold or flu, can lead to the production of excess mucus and cause the blood vessels in the nasal passages to become dilated, leading to congestion. Similarly, bacterial infections like sinus infections or streptococcal throat infections can also contribute to nasal congestion through inflammation and an increased production of mucus. Understanding the pathophysiology of nasal congestion helps shed light on the mechanisms behind these infectious causes and aids in the development of effective treatments and preventative measures.
Finally, understanding the pathophysiology of nasal congestion is crucial in determining the most effective treatment approach for relief. By delving into the specific underlying cause of this condition, healthcare professionals can tailor treatments to target the root issue and provide patients with long-lasting relief. Whether the nasal congestion is due to allergies, infections, or structural abnormalities, having a comprehensive understanding of the pathophysiology allows for a more informed and personalized approach. With this knowledge, patients can receive the most appropriate treatments, thereby improving their quality of life and alleviating the discomfort associated with nasal congestion.
Overview of Nasal Congestion:
The pathophysiology of nasal congestion is a complex process that involves the inflammation of the mucous membranes in the nasal passages. This common ailment often occurs as a result of various factors, such as allergies, colds, or the flu. When these mucous membranes become inflamed, they can swell, leading to a narrowing of the nasal passages and a disruption in the normal airflow. As a consequence, individuals may experience symptoms like difficulty breathing through the nose, a stuffy or blocked sensation, and an increased production of mucus. Understanding the pathophysiology of nasal congestion provides valuable insights into the underlying mechanisms and contributes to the development of effective treatments for this bothersome condition.
The pathophysiology of nasal congestion involves a range of factors that contribute to its onset and persistence. In addition to common causes like allergies and infections, certain environmental factors play a significant role in triggering nasal congestion. Smoke from tobacco or fires and various pollutants in the air can exacerbate nasal congestion symptoms. These external irritants have the potential to inflame the nasal passages, leading to swelling and increased mucus production. The body’s natural response to these harmful substances contributes to the obstruction of airflow and the feeling of nasal stuffiness. Understanding the impact of these environmental triggers is crucial in managing and preventing nasal congestion for individuals affected by this condition.
The severity of symptoms experienced in patients with nasal congestion can vary, ranging from mild discomfort to severely impaired breathing. Such variations are influenced by the diverse underlying causes and accompanying illnesses that contribute to the pathophysiology of nasal congestion. Understanding the intricate mechanisms involved in the pathophysiology of nasal congestion can shed light on the factors that exacerbate or alleviate symptoms. By exploring the complex interplay between anatomical abnormalities, allergic reactions, infections, or other contributing factors, healthcare professionals can tailor treatments to address the specific underlying causes and consequently alleviate the severity of symptoms. The study of the pathophysiology of nasal congestion, therefore, plays a crucial role in enhancing our understanding of this common condition and providing patients with appropriate care.
Finally, when considering the pathophysiology of nasal congestion, it is important to explore the various treatment options available. From over-the-counter medications that provide immediate relief, to more invasive procedures such as steroid injections or surgery in cases of chronic sinusitis or polyps blocking the airways, patients have a range of choices to find relief from this condition. By understanding the underlying mechanisms causing nasal congestion and the potential treatments available, individuals can make informed decisions about their own healthcare and seek appropriate medical intervention when necessary. The pathophysiology of nasal congestion is a complex process, but with proper evaluation and management, patients can find relief and regain control over their respiratory health.
Definition of Nasal Congestion
The pathophysiology of nasal congestion involves the inflammation of the nasal mucosa, which occurs due to an increase in blood flow and the accumulation of fluid in the sinus cavities. This condition leads to the obstruction of nasal airflow, causing the common symptoms of nasal congestion. The root cause is the inflammation, which triggers the increased blood flow and results in the accumulation of fluid. The inflammation is typically caused by various factors such as allergies, infections, or irritants. Allergies can trigger an immune response that causes the nasal mucosa to become swollen and produce excess mucus. Infections, such as the common cold or sinusitis, can lead to an inflammatory response in the nasal passages. Additionally, irritants such as pollutants or strong odors can also cause nasal congestion by irritating and inflaming the nasal mucosa. These factors disrupt the normal function of the nasal passages, leading to the blockage of airflow and the associated discomfort. To alleviate nasal congestion, it is important to address the underlying cause and reduce inflammation. This can be achieved through various treatment options such as antihistamines for allergies, decongestants to reduce swelling, and nasal irrigation to flush out excess mucus. Overall, understanding the pathophysiology of nasal congestion helps in identifying appropriate management strategies to alleviate this common condition.
The pathophysiology of nasal congestion involves various factors that contribute to the obstruction of airways. One of the primary causes is allergies, which trigger an immune response leading to inflammation and swelling of the nasal passages. Infections, such as the common cold or sinusitis, can also result in congestion as the body fights off the invading pathogens. Additionally, anatomical abnormalities like deviated septum or nasal polyps can narrow the airways, restricting proper airflow. Environmental factors play a role too, as exposure to cold air and pollutants can irritate the nasal lining and cause congestion. Overall, the interplay between allergies, infections, anatomical abnormalities, and environmental factors contributes to the development of nasal congestion, disrupting normal breathing processes.
Additionally, understanding the pathophysiology of nasal congestion is crucial in comprehending the negative impact it can have on an individual’s daily life. As mentioned earlier, common symptoms associated with this condition include a feeling of fullness in the nose, a lost sense of smell, post-nasal drip, difficulty breathing through the nose, and frequent headaches. Knowledge of these symptoms allows healthcare professionals to identify and diagnose nasal congestion promptly. It is essential to recognize that these symptoms stem from an underlying inflammatory process within the nasal passages, leading to increased mucus production and congestion. By grasping the pathophysiological mechanisms at play, medical interventions can be tailored to provide relief and improve the overall quality of life for individuals suffering from nasal congestion.
Symptoms of Nasal Congestion
The pathophysiology of nasal congestion involves a variety of factors that contribute to the experience of a stuffy nose and difficulty breathing through the nasal passages. This condition not only hampers the ability to breathe properly, but it can also disrupt sleep patterns and cause a temporary loss of smell or taste. The underlying mechanisms behind nasal congestion revolve around the inflammation and swelling of the nasal tissues, often triggered by various allergens and irritants. This inflammatory response leads to an increase in mucus production, causing further blockage of the nasal passages. Additionally, the dilation of blood vessels in the nasal cavity further exacerbates congestion. Various conditions such allergies, sinus infections, or structural abnormalities may contribute to the pathophysiology of nasal congestion. Understanding the intricate pathophysiological processes at play can aid in developing effective treatments and management strategies for individuals suffering from this common ailment.
The pathophysiology of nasal congestion is characterized by various symptoms that individuals may experience. Among these symptoms, patients may also notice the presence of postnasal drip, which refers to the sensation of thick mucus dripping down the back of their throat. This can lead to discomfort and irritation, further contributing to the overall effects of nasal congestion. Additionally, coughing may be another noticeable symptom that patients may encounter. As a result of the congestion, patients may experience an urge to cough in order to alleviate their discomfort. Finally, a sore throat may also accompany nasal congestion, causing patients to experience pain and irritation in their throat. Understanding the pathophysiology of nasal congestion allows for a comprehensive examination of these related symptoms and aids in the effective management of this condition.
Meanwhile, understanding the pathophysiology of nasal congestion is crucial for identifying and addressing its underlying causes. When faced with nasal congestion, it is imperative to consider various factors such allergies, cold, flu, sinus infections, or even structural issues like a deviated septum. By acknowledging the role these factors play in contributing to nasal congestion, individuals can take more informed steps towards finding effective relief and management strategies. Furthermore, recognizing the diverse etiologies and their impact on nasal congestion can help healthcare professionals tailor treatment plans to meet the specific needs of each individual. Overall, by delving into the pathophysiology of nasal congestion and exploring the range of possible causes, we can work towards alleviating the discomfort and inconvenience associated with this common condition.
Pathophysiology of Nasal Congestion:
The pathophysiology of nasal congestion is a complex process that encompasses various underlying conditions. One common cause is allergies, triggering inflammation in the nasal passages. This inflammation leads to the swelling of the nasal tissues and an increase in mucus production, ultimately causing a stuffy nose. Additionally, a cold virus can also be responsible for the inflammation and subsequent congestion. The viral infection prompts an immune response in the nasal passages, resulting in the same cascade of events. In either case, the inflamed nasal passages interfere with normal airflow, leading to discomfort and difficulty in breathing through the nose. Understanding the pathophysiology of nasal congestion provides valuable insights into its causes and mechanisms, aiding in the development of effective management strategies for individuals experiencing this bothersome symptom.
The pathophysiology of nasal congestion involves the inflammation of nasal passages, leading to various detrimental effects. When the nasal passages become inflamed, they narrow, creating an obstruction that hinders the free flow of air through the nose. This obstruction causes difficulty in breathing, resulting in a feeling of discomfort and compromised respiratory function. Moreover, the obstruction also affects the senses of smell and taste, impairing these essential faculties. Individuals experiencing nasal congestion may find it harder to perceive aromas or fully enjoy the flavors of food. The pathophysiology of nasal congestion showcases how this condition disruptively impacts multiple aspects of daily life, highlighting the significance of understanding and addressing it.
The pathophysiology of nasal congestion involves an inflammatory response in the nasal passages leading to the common symptoms of stuffiness and difficulty breathing through the nose. However, there are various treatment options available to alleviate these symptoms. Antihistamines, decongestants, steroids, and saline sprays are among the medications that can provide relief. By targeting the inflammation in the nasal passages, these medications help to reduce swelling and open up the airways, allowing for improved airflow. Antihistamines are effective in blocking histamine, a chemical responsible for triggering allergy symptoms. Decongestants work by constricting blood vessels in the nasal passages, reducing swelling and congestion. Steroids, such corticosteroids, have potent anti-inflammatory properties and can help manage more severe cases of nasal congestion. Saline sprays, on the other hand, provide a natural approach by moisturizing and rinsing the nasal passages, relieving congestion and promoting better breathing. These treatments provide individuals with options to effectively manage their nasal congestion and improve their overall quality of life.
Additionally, understanding the pathophysiology of nasal congestion is crucial in effectively managing its symptoms. While medications play a significant role in providing relief, incorporating lifestyle changes can further enhance overall symptom management. By avoiding triggers such pet dander or dust, individuals can minimize the likelihood of congestion episodes. Additionally, using a humidifier can help maintain optimal moisture levels in the nasal passages, preventing excessive dryness and reducing congestion. By realizing the underlying mechanisms of nasal congestion and implementing appropriate measures, individuals can take proactive steps towards alleviating this bothersome condition and improving their overall quality of life.
Anatomy of the Nose and Sinuses
The pathophysiology of nasal congestion is a complex phenomenon that involves various parts of the nose. The nose itself is made up of several different components, such the nasal vestibule, the nasal cavity proper, and the paranasal sinuses. Understanding the role of each of these structures is vital in comprehending the underlying mechanisms behind nasal congestion. The nasal vestibule serves the purpose of filtering and humidifying the inhaled air, while the nasal cavity proper consists of turbinates that help increase the surface area for air warming and moistening. Additionally, the paranasal sinuses are interconnected hollow spaces that contribute to the production of mucus and influence the airflow through the nose. By examining the pathophysiology of nasal congestion, we can better grasp how factors such inflammation, allergies, or infections disrupt these delicate processes and lead to the uncomfortable and obstructed nasal passages.
Nasal congestion, a common symptom of various pathophysiological conditions affecting the nasal cavity, is a bothersome and uncomfortable experience for many individuals. In order to understand the underlying mechanisms of nasal congestion, it is important to explore the anatomy of the nasal cavity. The nasal cavity proper, a key component of the respiratory system, is divided into three distinct sections: the superior meatus, the middle meatus, and the inferior meatus. These divisions play a crucial role in the regulation of airflow and the overall functioning of the nasal passages. When pathological conditions arise, such keywords associated with nasal congestion, such areas may become compromised leading to a disruption in normal breathing patterns. Understanding the relationship between these sectional divisions and nasal congestion can provide valuable insights into the management and treatment of this common symptom.
The pathophysiology of nasal congestion involves the understanding of various spaces within the nasal cavity. These spaces, which include the nasal passages and sinuses, are lined with a mucous membrane. This membrane plays a crucial role in maintaining the health and function of the respiratory system. It contains numerous blood vessels that aid in regulating temperature and humidity. This regulation ensures that the air entering the lungs remains moist, creating an optimal environment for proper respiratory function. However, in cases of nasal congestion, this delicate balance may be disrupted. Factors such inflammation, allergies, or infections can lead to an excessive production of mucus or swelling of the nasal tissues. These disruptions can impede the normal flow of air through these spaces, resulting in nasal congestion. Understanding the pathophysiology of nasal congestion allows for targeted interventions to alleviate symptoms and restore proper respiratory function.
All in all, understanding the pathophysiology of nasal congestion is crucial in comprehending the underlying mechanisms that contribute to this uncomfortable condition. As discussed, nasal congestion occurs when excess fluid accumulates in the nasal passage, obstructing the free flow of air. This is often caused by increased blood flow to the area, leading to the engorgement and swelling of the nasal blood vessels. Additionally, these blood vessels can become dilated due to inflammation or other causes, resulting in further nasal congestion. By recognizing these key factors, healthcare professionals can develop targeted interventions and treatments aimed at alleviating symptoms and improving the overall well-being of individuals suffering from nasal congestion.
Understanding Inflammation and Its Effects on the Nose and Sinuses
The pathophysiology of nasal congestion involves the body’s inflammatory response, which is a crucial mechanism for self-protection and healing. In this process, inflammation can occur within the nose and sinuses, leading to various symptoms including tissue swelling, increased mucus production, and increased mucosa permeability. Nasal congestion is a result of these inflammatory changes, often caused by factors such allergies, infections, or irritants. This condition disrupt patients’ respiratory function, causing discomfort and difficulty breathing. Understanding the pathophysiology of nasal congestion helps in developing effective treatment strategies to alleviate symptoms and improve patients’ quality of life.
The pathophysiology of nasal congestion involves the progressive inflammation of nasal and sinus tissues, which subsequently increases their susceptibility to obstruction. This obstruction is primarily caused by the swelling and narrowing of the nasal passageways. As a result, individuals experience symptoms such congestion, making it difficult to breathe comfortably. Furthermore, post-nasal drip becomes a common occurrence, leading to a constant sensation of mucus dripping down the back of the throat. These physiological changes significantly impact an individual’s overall quality of life, restricting their ability to perform daily tasks and affecting their general well-being. Understanding the pathophysiology of nasal congestion is crucial in finding effective treatments to alleviate its symptoms and improve patients’ comfort and functionality.
Next, it is crucial to recognize the potential long-term consequences of inflammation on the nasal passages and sinuses, particularly in relation to the pathophysiology of nasal congestion. Prolonged inflammation can lead to chronic sinusitis or upper respiratory infections, which often necessitate medical intervention and the use of medication to effectively manage the condition. Understanding how inflammation impacts these vital structures allows individuals to take proactive measures, such
as timely medical attention or appropriate medication, to mitigate the risks associated with prolonged inflammation. By being aware of the pathophysiology of nasal congestion and its potential complications like chronic sinusitis or upper respiratory infections, individuals can take steps to alleviate discomfort and prevent further health issues.
Common Causes of Nasal Congestion:
The pathophysiology of nasal congestion encompasses various common causes such allergies, cold, and sinus infections. When individuals experience these conditions, inflammation of the nasal passages occurs, leading to the production of excess mucous and subsequent swelling. As a result, the airflow through the nasal passages becomes obstructed. Allergies, triggered by specific substances such pollen or pet dander, can provoke an immune response in the nasal passages, causing inflammation and congestion. Colds are viral infections that irritate the nasal tissues, leading to congestion and mucous production. Sinus infections can be bacterial or viral in nature and cause inflammation in the sinuses, leading to nasal congestion. Understanding the pathophysiology of nasal congestion involves recognizing the role of inflammation, mucous production, and swelling in obstructing airflow through the nasal passages.
The pathophysiology of nasal congestion involves various factors such exposure to irritants and weather changes. Irritants like cigarette smoke or strong odors can trigger inflammation in the nasal passages, leading to congestion. This occurs when the nasal tissues become inflamed and swollen, restricting airflow. Similarly, weather changes can also play a role in nasal congestion due to a decrease in air pressure. This change in pressure can cause swelling in the tissues lining the nose, further contributing to congestion. Overall, understanding the pathophysiology of nasal congestion helps to highlight the impact of irritants and weather on the development of this common condition, emphasizing the importance of avoiding triggers and managing symptoms effectively.
Moreover, understanding the pathophysiology of nasal congestion requires acknowledging that it can be caused by a range of factors, including structural issues. Deviated septum and enlarged adenoids, among other structural abnormalities, can lead to blockages in the nasal passages, resulting in difficulty breathing through the nose and persistent congestion. By recognizing these underlying causes, healthcare professionals can effectively diagnose and treat individuals suffering from nasal congestion. Treatment options can vary, from medication to surgical interventions, depending on the severity of the structural issues. Overall, a comprehensive understanding of the pathophysiology of nasal congestion is crucial for providing targeted and effective therapeutic interventions to alleviate symptoms and improve the quality of life for affected individuals.
Allergens
The pathophysiology of nasal congestion revolves around the body’s immune system response to allergens, which can lead to significant discomfort. When exposed to allergens, such as pollen or dust mites, the immune system recognizes them as threats and releases histamines. These histamines trigger an inflammatory response in the nasal passages, resulting in swelling and congestion. This process is a crucial part of the body’s defense mechanism, intended to trap and eliminate potential allergens. However, in individuals with allergies or sensitivities, this immune response can become exaggerated and lead to persistent nasal congestion. Understanding the pathophysiology of nasal congestion provides insight into the intricate mechanisms that contribute to this common symptom, allowing for targeted treatment options to alleviate discomfort and improve overall quality of life.
Nasal congestion, a common symptom experienced by many individuals, is primarily caused by inflammation within the nasal passages. This inflammation disruptively leads to swelling around the sensitive mucous membranes present in the nose. As a result, the once freely flowing airflow becomes restricted, leading to a feeling of congestion. This reduced airflow causes discomfort and difficulty in breathing through the nose. When examining the pathophysiology of nasal congestion, it becomes evident that the inflammatory response plays a significant role in this condition. Understanding the underlying mechanisms of this inflammation is crucial in finding ways to alleviate the discomfort and restore normal nasal function for those affected.
However, understanding the pathophysiology of nasal congestion can shed light on the underlying mechanisms that lead to this bothersome symptom. In the case of allergens such dust, pollen, pet dander, mold spores, and certain foods, nasal congestion occurs when these substances come into contact with the sensitive lining of the nasal passages. This triggers an immune response, characterized by the release of histamines and other inflammatory mediators. Consequently, blood vessels in the nasal mucosa become engorged, leading to swelling and increased mucus production. As a result, the individual experiences a blocked or stuffy nose. By recognizing the role of these common allergens and their impact on the physiology of nasal congestion, healthcare professionals can better tailor treatment plans, offering relief and improving quality of life for those affected by this condition.
Environment Factors
The pathophysiology of nasal congestion can be attributed to various environmental factors. Cold temperatures, for instance, can have a significant impact on the nasal passages. When exposed to cold weather, the lining of the nose can become irritated and inflamed, leading to congestion. Similarly, low humidity levels can also contribute to this condition by drying out the nasal passages, causing discomfort and congestion. Additionally, air pollution is another significant factor that can exacerbate nasal congestion. The presence of pollutants in the air can irritate the nasal lining, causing inflammation and blockage. Understanding the role of these environmental factors in the pathophysiology of nasal congestion helps shed light on the mechanisms by which such conditions occur.
The pathophysiology of nasal congestion involves an inflammatory response that leads to the swelling of tissues in the nose. This inflammation causes a narrowing of the nasal passages, resulting in the frustrating experience of blocked nostrils. Additionally, this process leads to the trapping of excess mucus, further adding to the discomfort. Understanding the intricate mechanisms behind the pathophysiology of nasal congestion can help in developing effective treatments and alleviating the symptoms associated with this condition.
The pathophysiology of nasal congestion involves various factors, one of which is the presence of allergens in the air. These allergens, such pollen or dust mites, can trigger an allergic reaction when they come into contact with the nasal passages. This reaction leads to increased swelling and irritation in the nasal linings, causing the sensation of congestion. Additionally, the body’s immune response to these allergens results in an increased production of mucus, further contributing to the blockage and discomfort in the nose. The nasal congestion caused by allergens can be particularly bothersome and can significantly impact an individual’s quality of life. Therefore, it is crucial to identify and manage the underlying allergens to alleviate symptoms and promote better nasal health.
Thus, it is evident that understanding the pathophysiology of nasal congestion is crucial to comprehending the various factors that contribute to this uncomfortable condition. While direct irritation from environmental factors can be a primary cause, it is important to recognize that changes in air pressure can also play a significant role in the swelling of nasal passages and subsequent congestion. By delving deeper into the intricate mechanisms of nasal congestion, researchers and medical professionals can further develop effective treatment strategies and preventive measures to alleviate the symptoms associated with this common health issue.
Viruses/Bacteria/Fungi
The pathophysiology of nasal congestion involves the inflammatory response triggered by certain viruses, namely the cold, flu, and acute respiratory tract infections. These viral pathogens invade the nasal passages and prompt an immune response, leading to inflammation and subsequently causing congestion. The body’s defense mechanisms perceive these viruses as foreign invaders and release various chemicals, such as histamines and leukotrienes, which induce blood vessel dilation and increased blood flow to the nasal tissues. Consequently, the nasal passages become swollen, resulting in a blocked or stuffy nose. This physiological response is the body’s attempt to contain and eliminate the viral infection. Overall, understanding the pathophysiology of nasal congestion helps us grasp how viral illnesses impact our respiratory system, highlighting the importance of proper preventive measures and healthcare interventions to alleviate symptoms and promote recovery.
The pathophysiology of nasal congestion involves various factors, one of which is bacterial infections. Bacterial infections can contribute to nasal congestion by causing inflammation in the mucous membranes of the upper respiratory system. When these bacteria inflame the mucous membranes, it leads to a blockage and swelling of the nasal passages, resulting in difficulty breathing through the nose. In addition to bacterial infections, other factors such as allergies, sinusitis, and structural abnormalities can also play a role in the pathophysiology of nasal congestion. Understanding the pathophysiology of nasal congestion is crucial for effective treatment and management of this common condition.
Meanwhile, understanding the pathophysiology of nasal congestion is crucial to managing the various underlying causes, including fungal infections like sinusitis. Such infections can lead to inflammation of the sinuses, resulting in nasal obstruction and congestion. By recognizing the mechanisms involved in this process, healthcare professionals can better tailor treatment strategies for patients, aiming to alleviate their symptoms and improve their quality of life. With further research and advancements in our understanding of the pathophysiology of nasal congestion, more targeted and effective interventions can be developed, ultimately bringing relief to those who suffer from this common condition.
Structural Abnormalities or Irritants in the Nose & Sinuses
The pathophysiology of nasal congestion involves the presence of structural abnormalities in the nose and sinuses. Two common causes are a deviated septum and a nasal polyp. These abnormalities disrupt the normal airflow and can result in nasal congestion. When the nasal passages become blocked or narrowed, it becomes challenging for air to pass through smoothly. As a consequence, individuals experience difficulty breathing through the nose. Understanding the pathophysiology of nasal congestion provides insights into the underlying mechanisms that contribute to this condition, aiding in diagnosis and potential treatment strategies.
The pathophysiology of nasal congestion involves the role of irritants in triggering this condition. Various irritants, including dust, mold, smoke, and pollen, can enter the nose and sinuses, causing irritation and inflammation. This irritation prompts the body’s natural response to produce excess mucus in an attempt to flush out these irritants. However, this excessive mucus production leads to a buildup of mucus in the nasal passages and sinuses, resulting in nasal congestion. The pathophysiology of nasal congestion highlights how the body’s protective mechanism can sometimes contribute to the discomfort experienced by individuals.
Thereafter, understanding the pathophysiology of nasal congestion is crucial in comprehending the multifaceted nature of this common ailment. It is evident that nasal congestion arises from a complex interaction of various factors, such
as increased blood flow, enlarged blood vessels, nasal tissue swelling, and excessive mucus production. Furthermore, the pathophysiology of nasal congestion involves both structural and environmental irritants that trigger inflammation in the nose and sinuses. This inflammatory response not only exacerbates nasal congestion but also contributes to the development of accompanying symptoms. By recognizing and addressing the underlying mechanisms at play in the pathophysiology of nasal congestion, healthcare professionals can employ more targeted and effective treatment strategies, offering patients relief and improved quality of life.
Medications or Drug Use
The pathophysiology of nasal congestion is a complex process that can often be linked to the use of specific medications. Nasal congestion, characterized by a stuffy or blocked nose, is frequently associated with the intake of certain over-the-counter decongestants, nasal sprays, and antihistamines. These medications, although commonly used to alleviate nasal congestion symptoms, can contribute to the underlying mechanisms of this condition. Decongestants work by constricting blood vessels in the nasal passages, which helps to reduce swelling and open up the airways. However, prolonged or excessive use of decongestants can lead to a phenomenon known colloquially “`rebound congestion“` or medical term “`rhinitis medicamentosa“`. Similarly, nasal sprays containing medications such “`oxymetazoline“` or “`phenylephrine“` can provide temporary relief by shrinking blood vessels and reducing inflammation. Nevertheless, when used for more than a few days, these sprays can cause a rebound effect, leading to worsened nasal congestion over time. Furthermore, antihistamines, which are commonly used to treat allergies, can also contribute to nasal congestion due to their drying effect on the nasal passages. In summary, although these medications offer initial relief, they can inadvertently exacerbate the pathophysiology of nasal congestion if used improperly or for extended periods.
Read also: Chronic Rhinosinusitis Pathophysiology
The pathophysiology of nasal congestion is a complex and multifaceted process. One important aspect to consider is the potential impact of long-term use of certain medications. While these medications are initially designed to alleviate symptoms, their continuous use can lead to an unforeseen consequence. Specifically, these medications may have the opposite effect and exacerbate congestion. This occurs due to the irritating nature of the medication on the nasal lining, which can cause inflammation and further constriction of the airways. Additionally, these medications can interfere with the protective mucus layer in the nose, reducing its effectiveness in trapping and removing irritants. Thus, although these medications may provide temporary relief, it is crucial to be aware of their potential long-term implications for nasal congestion.
Meanwhile, it is important to recognize that the pathophysiology of nasal congestion extends beyond the commonly known causes such allergies and the common cold. The effects of drugs such cocaine, marijuana, and other stimulants on blood vessels in the nose can also contribute to this condition. When these substances are used, the blood vessels in the nasal passages become inflamed and swollen, leading to a blockage of the airway. This not only creates discomfort for individuals but can also have significant implications for their overall health. Understanding the underlying mechanisms and pathways involved in the pathophysiology of nasal congestion caused by drugs is crucial in order to develop effective treatments and interventions that address this issue comprehensively.